Knee osteoarthritis is so common that it has its own name: gonarthrosis. Another name for this disease is deforming arthrosis.
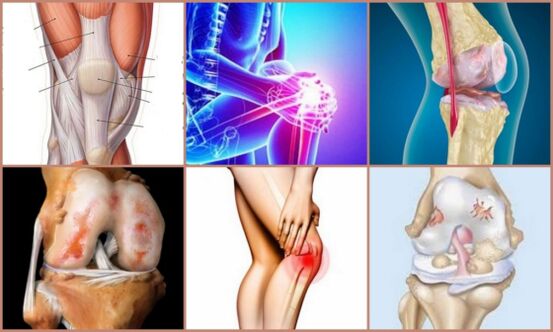
Osteoarthritis of the knee joint worries 20% of the population, its ICD-10 code is M17. Half of knee diseases are due to osteoarthritis. This is a disease in which the tissue of the cartilage and joint surface degenerates - they break down. The joint is poorly supplied with nutrients and oxygen, its function deteriorates and inflammation occurs. It becomes inactive and painful, and the patient's quality of life decreases. Complications of osteoarthritis lead to a wheelchair.
Let's find out what arthrosis of the knee joint is and how to treat it. How can the disease be prevented and how dangerous is it?

Causes and classification
The causes of arthrosis of the knee joint are different - mechanical damage, hereditary predisposition, metabolic disorders.
The occurrence of the disease is accompanied by excessive strain on the knees. In many sports, this is an accident at work. People with a high degree of obesity, over 60 years old, almost always suffer from arthrosis of one degree or another due to constant microtraumas. Osteoarthritis is an occupational disease in areas where a person has to stand for long periods of time or lift heavy objects. The disease can begin after rheumatoid arthritis.
The most common cause of knee osteoarthritis is injury. The second most common is childhood dysplasia. Inflammation due to autoimmune diseases is the third source of osteoarthritis. There are usually several reasons, one complementing the other.
Types of arthrosis of the knee joint, depending on the cause, are divided into primary and secondary. If the etiology is unknown, it is referred to as primary osteoarthritis; if the cause is clear, it is referred to as secondary osteoarthritis.
Development mechanism
The cartilage is nourished by constant changes in osmotic pressure. When the joint is loaded, the viscosity of the intra-articular fluid decreases and its quantity increases. When at rest, the intra-articular fluid becomes viscous and the amount decreases. Normally these processes alternate. The cartilage plate acts as a pump and pushes fluid out of the joint when it is stressed and sucks it back in when it relaxes. This is how the joint tissue is nourished. The pathological process manifests itself when the joint is exposed to destructive influences:
- If the load is large and the joint does not have time to recover, a nutritional disorder occurs. The cartilage becomes thinner, cracks and ulcers appear;
- The structure of the collagen fibers is disturbed and they absorb more poorly. Cartilage and kneecap become softer, less elastic and perform their functions more poorly;
- Bone growths appear in the joint. The membrane of the joint capsule becomes irritated and inflamed;
- As a person begins to take care of their knee and move little, less intra-articular fluid is produced. The surface of the cartilage becomes dry and rough;
- The knee receives even less nutrition, atrophies and its destruction accelerates.
Signs of arthrosis of the knee joint appear: it becomes inactive and pain appears. The pain is particularly severe in the morning and after prolonged immobility.
Stages of osteoarthritis
There are three degrees of osteoarthritis:
- Initial phase. The tissue is not yet destroyed. So far, only the function of the synovial membrane has deteriorated. The composition of the intra-articular fluid has changed. The knee can no longer withstand normal stress;
- Articular cartilage and menisci begin to deteriorate. Osteophytes – bone structures – grow into the bones. Inflammation and pain occur;
- Difficult stage. The support platform of the knee joint is deformed and the axis of the leg changes. The ligaments shorten and the joint capsule becomes stiff. The joint is pathologically mobile, but it is impossible to fully flex or straighten it. Inflammation and pain are pronounced.
On a note!
At the beginning of the disease, the muscles are intact. Their function is gradually lost. In the third stage, movement is severely restricted. By changing the axis of movement, the muscle attachment points change. The muscles are deformed - they contract or stretch, they can no longer contract normally. The nutrition of the entire leg tissue suffers.
Symptoms
Symptoms of arthrosis of the knee joint at the beginning of the disease do not make themselves felt in any way and do not force the patient to consult a doctor. The patient notices fatigue and pain, but does not attach serious importance to them.
The classic sign of knee osteoarthritis is immobility and stiffness in the joint, a pulling sensation in the back of the knee, and pain after exertion. It is difficult to move in the morning or after long periods of immobility. Relief occurs when the patient stretches his knee, massages it, and walks around.
After some time, the intensity and duration of the pain increases. A crunch appears in the joint, bending and bending completely stops. When walking, a person begins to limp - most patients come to the doctor with this complaint. Treatment for osteoarthritis of the knee joint usually only begins in the second stage.
If nothing is done, movement is only possible with outside help. When the patient lies down, the knee hurts less, but the pain is often annoying at night.
In the second and third stages, the knee joint is deformed - the contours of the bones are sharply defined, the lower leg is curved. If you place your hand on your knee, you will hear a crunching sound as it bends and straightens. When the kneecap moves, it also creaks. Fluid collects in the cavity, the joint swells and the tissue bulges.
As the disease progresses, all symptoms worsen.

diagnosis
The diagnosis of arthrosis of the knee joint is carried out comprehensively: an anamnesis is taken, laboratory and instrumental methods are prescribed.
inspection
The doctor examines the damaged joint, measures the bones and the flexion angle and determines the degree of mobility of the joints at the angle.
Analyzes
The patient is sent for a general blood test, a biochemical blood test and a general urinalysis.
roentgen
An x-ray of the knee joint is the most important source of information for making a diagnosis. Osteoarthritis of the knee joint can be seen in the photo: the joint space is narrowed, the cartilage is sclerotic, the bones are damaged; Joint deformation, salt deposition and dystrophic changes occur. Osteophytes can be clearly seen in the image.
Good to know!
In the case of osteoarthritis of traumatic origin, x-rays have a high diagnostic value and must be carried out without fail.
Ultrasonic
Ultrasound diagnostics is a meaningful method. Ultrasound does not replace X-rays and does not provide an image of the type of destructive process in the joint.
MRI
Magnetic resonance imaging provides a complete picture of the disease. This is a modern and precise research method that enables early diagnosis. The disadvantage of MRI is its high cost.
Treatment
Treatment of the knee joint for osteoarthritis is carried out on an outpatient basis and hospitalization is not necessary.
Treatment regimen:
- Reduce the load as much as possible;
- Follow the prescribed traffic regulations;
- Perform therapeutic exercises.
The aim of treatment is to slow down the destruction process, prevent contractures (the inability to fully bend and straighten the leg) and, if possible, restore the function of the joint. During the rehabilitation period, staying in sanatoriums and health resorts shows good results.

Drugs
Only the doctor decides on the treatment of osteoarthritis of the knee joint. You cannot choose medications yourself.
Inflammation is relieved with NSAIDs (non-steroidal anti-inflammatory drugs).
Good to know!
Because arthritis causes severe pain, NSAID injections provide quick action and a feeling of relief.
In modern treatment of knee arthrosis, NSAIDs from a different group are used. Their effect is more pronounced.
If there is inflammation of the joint mucosa, the doctor prescribes corticosteroid hormones for intra-articular administration. Hydrocortisone, Kenalog and Diprospan relieve inflammation and pain, but have many contraindications.
If necessary, antienzyme substances are injected into the joint cavity – Contrical, Ovamine, Gordox. They can significantly slow down the destructive process.
Intra-articular injections of hyaluronic acid and its preparations are also prescribed. It restores the protective and shock-absorbing properties of the synovial fluid.
Chondroprotectors are commonly prescribed, but there is no evidence that they help.
physical therapy
The latest methods of treating knee osteoarthritis do not exclude proper loading. The goal of physical therapy is to provide the necessary amount of movement while not overloading the joint and maintaining balance. If the patient does not understand how to treat arthrosis of the knee joint - when it is necessary to protect and develop the knee at the same time, the result of other methods is greatly reduced or reduced to zero. It is possible to get rid of the disease if the patient is conscious.
Laser therapy and physiotherapy
Laser treatments and physiotherapeutic procedures have proven to be excellent, especially when they can be used in the first stage.
Other methods
Intraosseous blockages have a therapeutic effect and interrupt the inflammatory cycle. In addition to the blockade, multichannel electromyostimulation with a special device is used.
Compresses made from homemade ointments and rubs can relieve pain and swelling.
prosthetics
If necessary, an operation is carried out - the patient is provided with a knee joint endoprosthesis. Modern prosthetic methods enable patients to return to sport.

Alternative and traditional medicine
Proponents of the unconventional approach argue that only with their methods is it possible to eliminate symptoms and treat arthrosis of the knee joint - without resorting to medication. These are exercise therapy (a special set of exercises), ozone therapy (physiotherapy with ozone injected into the joint), homeopathy, treatment with nutritional supplements, manual therapy, massage.
Attention!
If you use unconventional methods, you must remember that their effectiveness has not been proven.
There are original methods of treatment, but reviews about them vary.
Rehabilitation and prevention
Only therapeutic exercises and a measured load on the joint can restore the knee joint in osteoarthritis. If the patient follows all the doctor's recommendations and is ready to fight for his health by all means, the answer to the question "Can arthrosis of the knee joint be cured" is positive in most cases.
Prevention consists in timely assistance with injuries, active exercise without overload and maintaining an optimal body mass index.
Patient opinions
Reviews of patients who have undergone traditional treatment are usually positive, but there are also negative ones.
When making a final decision about treatment, you should consult your doctor without forming an opinion based on reviews.
Medicine has learned to successfully treat joint diseases, the consequences of which inevitably led to disability in the last century. If you have osteoarthritis of the knee joint, it is important to seek help in a timely manner in order to determine the stage of the disease and the extent of treatment.
























